Clinical Services
Hysterectomy
Mr Fayyad is one of few Gynaecologists in the UK providing Total Laparoscopic Hysterectomy as a one night stay procedure. This guarantess treatment of heavy and/or painful periods in a minimally invasive way. The operaston is performed through key-hole surgery and the patient is discharged home next day. Return to work and driving is usually within 14 days.
For a video of Total Laparoscopic Hysterectomy, please visit the following link:
Urinary Incontinence:
Urinary incontinence in women (leakage) refers to the involuntary loss of urine from the bladder, which constitutes a social or hygienic problem for the individual. Bladder control problems affect about 17 million people in the United States. It can be a cause of anxiety, social embarrassment and may limit ones social and daily activities. Fortunately, most of these conditions can be treated. However the first step to curing this condition is acknowledging the problem and then deciding to see a physician who has been properly trained in treating the condition of incontinence.
Incontinence Causes
There are two main types of urinary incontinence: Stress incontinence when leakage is associated with activity including coughing, sneezing, and exercise. The other type is overactivity incontinence, where incontinence is associated with urgency, urinary frequency and getting up at night to pass urine.
There are many causes of urinary incontinence. Some of the causes of incontinence are related to temporary conditions. Once they are treated, the incontinence usually goes away. Temporary causes include:
-
Urinary Tract Infection
-
Constipation
-
Certain medications
-
Increased dietary intake of caffeine, alcohol, artificial sweeteners and carbonated beverages
-
Some other causes of incontinence are not temporary. There is, however, treatment available for many of these conditions. Other causes of incontinence include:
-
Weakness of the muscles that hold the bladder in place
-
Weakness of the bladder sphincter muscles
-
Overactive or under active bladder muscles
-
Neurological disorders (EX: Multiple Sclerosis, Parkinson's Disease, Stroke)
Stress Incontinence Treatment
Conservative Therapy
Pelvic Floor Exercises (Kegel Exercises)
This is treatment for urinary incontinence which, when done faithfully and correctly, can help decrease the urgency a patient may have and help with both urge incontinence and stress incontinence. The pelvic floor muscle is like a hammock that stretches from the pubic bone in the front to the tailbone in the back. This set of muscles supports the organs of the pelvic region, which include the bladder, large intestines and uterus. Since this muscle is often not exercised, it is generally weak to begin with, which contributes to urinary symptoms. Childbirth will weaken this muscle more because during vaginal delivery, the child's head and body push under the pelvic floor muscle and stretches it extensively, which causes temporary additional damage/weakening. Learning to do these exercises can help with incontinence; however, to perform these incontinence treatment exercises effectively, the patient must first identify the correct muscles. Two methods of identifying the correct muscles:
-
While urinating stop the flow of urine by tightening the pelvic floor muscles. Do not perform the incontinence treatment exercises while urinating, since this can lead to difficulty in voiding. Stopping and starting the stream as a person voids is a popular misnomer and should not be done. Patients may elect to try to stop the stream once or twice to check for contraction of the correct muscle.
Place a finger in the vaginal opening and attempt to squeeze the finger. Upon squeezing, One key point is that patients do not want to use other muscles, such as the abdomen, legs or buttocks. While doing bladder incontinence treatment, it is important to isolate the muscles only to further increase their strength. If you are moving these muscles or holding your breath, you are probably trying too hard!
When performing incontinence treatments, concentrate just on the pelvic floor muscles and do the best you can. This contraction will get easier with practice. One exercise program is described below:
-
Identify the correct muscles that are to be exercised.
-
Attempt to contract and hold the muscle squeeze for 10 seconds
-
Relax for a period of 10 seconds
-
Perform 10-15 contractions and relaxation
-
Perform this regimen 3-4 times a day
It may take awhile to work up to a 10 second hold. In the beginning, you will probably not be able to hold for more than five or six seconds and that is all right. Between each contraction, relax for 10 seconds. This allows the muscle to rest adequately to be able to perform well for the next contraction. If you do not relax the muscle well enough, the muscles will tire quickly. By faithfully doing your Kegel exercises, you should see an improvement in your symptoms starting in four to six weeks.
Vaginal cones are sometimes used to help with pelvic floor exercises. Vaginal cones are miniature weights which are placed into the vagina and help women achieve stronger pelvic floor.
Urodynamics
"Uro" means urine or related to the urinary system. "Dynamics" means moving against pressure. Health professionals recommend patients have urodynamic testing so they can have a better understanding of how urine moves through your lower urinary system and how well the bladder is working.
The lower urinary system consists of the ureters, bladder, urethra and sphincter muscle. The bladder is a balloon-like organ with a muscular wall that expands and contracts (squeezes). Urine travels from the kidneys to the bladder through tubes called ureters. Urine is stored in the bladder until you decide to empty it. Emptying occurs by a contraction of the bladder muscle. This means that the bladder muscle "squeezes" to empty the urine.
The sphincter [SFINK-ter] muscle sits right below the bladder and is around the urethra (urine pipe). The bladder neck is a tube that connects your bladder to the urethra. The urethra opens to the outside of your body, where urine comes out. If you are not ready to empty your bladder, then the sphincter muscle tightens up, like a knot at the bottom of a water-filled balloon. When you decide that it is time to empty your bladder, the sphincter muscle relaxes (like untying the balloon) and urination starts.
The urethra opens to the outside of your body, where urine comes out. If you are not ready to empty your bladder, then the sphincter muscle tightens up, like a knot at the bottom of a water-filled balloon. When you decide that it is time to empty your bladder, the sphincter muscle relaxes (like untying the balloon) and urination starts.
Urination takes place only when muscles and nerves are working correctly. Messages are constantly being exchanged between the bladder and brain through a pathway of nerves in the spinal cord. Sometimes a head injury, stroke, or other diseases of the spine will cause problems with a nerve pathway. Then the bladder may not empty correctly. But your bladder may not empty correctly even if you do not have any of these problems. Persons sometimes have incontinence (leakage of urine) before and after having bladder, pelvic, or back surgeries. People may leak urine when they cough or sneeze, maybe they leak urine when they have the urge to go to the bathroom, and maybe they leak urine for no reason at all. That is why it is so important to have urodynamic testing, to show how well nerves and muscles are working and find a cause for your urine control or voiding problems. The urodynamic test takes about 1/2 hour. It will be done in the office. You can drink non-alcoholic, caffeine-free beverages or eat anything you want before the test, unless given other instructions by your health provider.
On the day you go to have the test done, make sure your bladder is comfortably full. Go to the bathroom as you normally would until about 2-3 hours before your appointment time. At that point do not urinate anymore and drink 3-4 (8-ounce) glasses of fluid. Any thing you prefer is fine but water is the best option. If you can't make it, RELAX it is not the end of the world. Go to the bathroom and bring a large jug of water with you in the car and drink on the way to the appointment.
You will be asked to empty your bladder into a special commode. This will record how well you urinate, and how strong your stream is. A small tube called a catheter will be inserted into your bladder. It is about the size of a regular piece of spaghetti. It may burn slightly or feel a little uncomfortable when it is in place, or it may not bother you at all. It will be used to fill your bladder with water and measure the change in bladder pressure as it fills and empties. A very small tube will be inserted into your vagina. You should not feel this at all. It will measure the pressure in your abdomen when you strain or cough. Two patches or tiny electrodes, similar to an EKG test, will be placed on each of your buttocks near your rectum. These will monitor any muscle movement and its ability to work properly when you wish to urinate. These may cause a little discomfort when coming off, like pulling off a Band-Aid. If you have prolapse (bulging in your vagina) it will be pushed back and held up in place during the testing. This too may be a slightly strange feeling, but it is important to do the testing with the bladder and vagina in a normal position.
As your bladder is filled with fluid through the catheter, you will be asked to describe how your bladder feels. You may be asked to strain or cough several times. When your bladder is full, you will empty it. The entire test will be recorded on a computer, and you may even be able to watch it on a screen as it is occurring. Everything should be explained to you by the health professional as the test is being performed.
The catheters will be removed when the test is over. You may have a little discomfort where the catheters were placed. It may burn slightly when you go to the bathroom; this should last only a few hours. A warm tub bath (with no bath additives) will help to ease any discomfort. Drinking an adequate amount of fluid-usually 4-6 (8-oz.) glasses-is important (especially water) within 24 hours after the test. This will help prevent a urinary tract infection. An oral antibiotic well be given to you after the test and you will take it as directed at home with food. You may continue your diet, medications, and activities as normal, unless given other instructions by your health professional. After 24 to 48 hours your should not have any discomfort from the test. If you have any burning with urination, the frequent need to go to the bathroom or the urgent feeling you need to get there quickly, please call the office (610 435-9575 ext. 102). You may need more antibiotics.
After the test, an appointment will be made with the doctor to explain his or her
Surgical treatment of stress urinary incontinence
There are numerous minimally invasive surgical treatments for stress urinary incontinence that Mr Fayyad offers his patients that include the tension free vaginal tape (TVT), and urethral bulking agents (Bulkamed) and key-hole surgery to suspend the bladder neck (laparoscopic colposuspension).
Tension-Free Vaginal Tape (TVT sling) Sling
The goal of surgery for stress urinary incontinence is to stop urinary leakage and this is accomplished by supporting the urethra. The urethra is the tube that allows urine to be expelled from the body. In an attempt to support the urethra, the vagina under and beside the urethra is the area which the operation takes place. This procedure is commonly called the SLING.
Mr Fayyad have been trained to perform a number of different types of sling operations utilizing various types of material, sutures and points of anchoring. Currently he chooses to offer their patients an extremely minimally invasive sling operation known as the TVT sling or tension free vaginal tape sling.
This TVT procedure has been performed in Europe for more than 12 years with great success. Mr Fayyad serves as a preceptor to teach this operation to Urologists, Urogynecologists and Gynecologists throughout the world. In August 2009, Mr Fayyad travelled to Jordan to introduce the TVT sling operation to his colleagues at the University of Jordan.
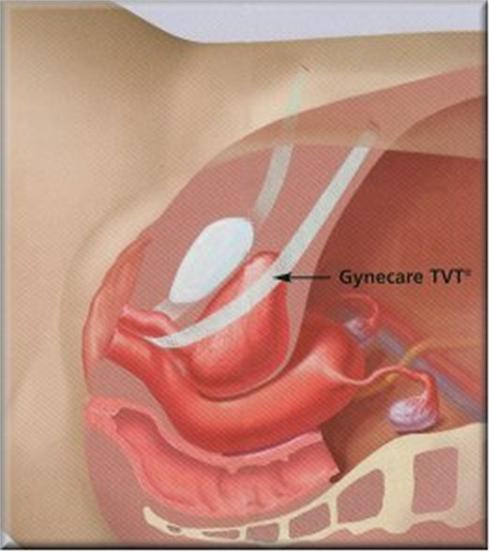
Figure 1

Figure 2: TVT sling
The operation has the following advantages:
-
Minimally invasive (two incisions of 1/3 inch on the pubic hairline)
-
Minimal pain (40% of patients will not need a pain reliever after 24 hours)
-
Proven cure rate of 86%
-
Same day or next day discharge for 98% of patients
-
Performed under local anesthesia and IV sedation
-
Operative time 20-30 minutes
-
Minimal postoperative need for catheterization
-
Minimal complications which include voiding dysfunction, mesh erosion and urinary urgency
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on mid urethral sling procedures.
Bulkamed Injections:
Collagen is a naturally occurring protein found in humans and animals and supports the closure mechanism of the bladder. When Bulkamed is injected into the tissue around the urethra, it adds bulk and helps it close tightly to prevent urine leakage, especially urine leakage associated with activity (Stress Urinary Incontinence). Most patients will leak much less or not leak at all after Bulkamed therapy. Some patients will need to have one or more injections done at a later date because the body will absorb some of the collagen material. The length of time between injections varies with each patient. Some need to be re-injected after a few months and some after a few years.
The procedure could be done under local, spinal (like epidural injection) or general anaesthetic. It is mostly suitable for elderly women who are not fit for more invasive treatments or women who had previous failed incontinence surgery.
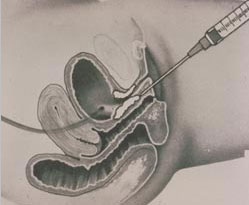
Incontinence Treatment: Figure 2
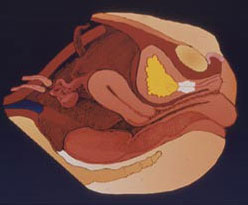
Incontinence Treatment: Figure 3
Overactive Bladder (OAB)
This is a common condition that has a significant impact on patient's life and is characterized by urinary urgency, which is a sudden compelling desire to pass urine, associated with increased urination frequency and nocturia (getting up at night to pass urine once or more). There are many causes of overactive bladder, including neurological conditions and diabetes, but in most cases, no significant cause can be found.
Treatment of overactive bladder (OAB)
The mainstay of the treatment of this condition include the use of medications called anti muscarinics to relax the bladder. These are tablets that are usually used once daily and help reduce the urgency and urgency incontinence. I also strongly advise patients to reduce caffeinated drinks intake (mainly tea, coffee, fizzy drinks and alcohol). In addition, patients will benefit from bladder retraining where the bladder is trained gradually to accomodate larger volumes of urine. Occasionally, patients need a special bladder test called urodynamics to diagnose the cause of incontinence and assess the continence mechanism and the function of the bladder muscle. For further information about urodynamics, please see the "Home Page".
If the above treatment fails, patients can be a candidate for intravesical botox treatment (injections into the wall of the bladder under anaesthetic).
Intravesical Botulinium Treatment (Botox)
This treatment is reserved for women with overactive bladder (OAB), with symptoms of urgency, frequency and urgency incontinence who failed to respond to conservative treatment, that includes fluid management, bladder retraining and medications. The procedure is quick and done as a day-case procedure. Patients can have either general anaesthetic, epidural anaesthetic, or local anaesthetic. A very fine needle is inserted into the bladder with the telescope (cystoscope), and Botox treatment is injected into 15-20 sites in the bladder wall. This treatment is very successful in treating women with overactive bladder symptoms with expected significant improvement in 80-90% of women. The treatment can result in slight problem in emptying the bladder in 10-20% of women that tends to resolve over time. Patients generally will need repeat treatments every 9-12 months to stop the symptoms coming back. Mr Fayyad is fully trained to provide this treatment for women with OAB, with excellent success rate, and day-stay procedure.
Painful Bladder Syndrome (Interstitial Cystitis)
This is a distressing condition with no known cause. Women classically present with pain in the lower abdomen when the bladder is full. It can be caused by recurrent infections in the bladder, and is diagnosed by cystoscopy (telescope examination of the bladder). The treatment involves tablet treatment for the pain and bladder instillation of cystistat (bladder medicine) to control the pain.
Pelvic Organ Prolapse
What is Pelvic Prolapse?
Pelvic prolapse is the loss of pelvic support that occurs when the soft connective tissue that support the pelvic organs become stretched, weakened or torn. It is a very common disorder, particularly in older women.
While aging is a factor, there are many potential contributing causes. They include loss of muscle tone, menopause and estrogen loss, multiple vaginal deliveries, obesity, uterine fibroids, family history, pelvic trauma or previous surgery, repeated heavy lifting, chronic constipation and coughing and certain medical conditions such as diabetes.
Did you know…
Half of all women over age 50 experience some degree of pelvic organ prolapse. Twenty percent of women over 60 years of age will require surgical intervention.
The symptoms of pelvic prolapse: Loss of bladder or bowel control, difficulty voiding, urinary frequency, problems with bowel movements, feelings of pelvic or vaginal heaviness, bulging.
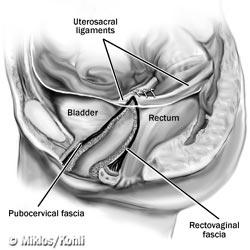
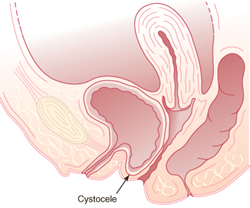
Anterior Vaginal Wall Prolapse (Cystocele and Urethrocele)
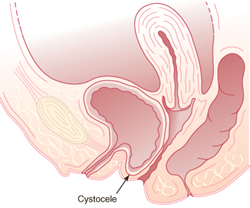
Figure 2: Diagramatic illustration of cystocoele

Figure 1: Cystourethrocoele
The anterior vaginal wall supports the bladder and the urethra. The anterior vaginal wall supportive layer is called the pubocervical fascia. Anterior vaginal wall is named based upon its two ends of attachment. Anterior vaginal wall is attached distally to the pubic bone area and proximally to the cervix if the uterus has not been removed. The pubocervical fascia is also attached laterally (on both sides) to the pelvic floor muscles specifically the obturator internus muscle. As long as this vaginal wall stays in place the bladder and urethra will stay in its normal anatomical position.
Patients with cystocele or cystourethrocele may experience:
-
Pelvic/Vaginal pressure
-
Dyspareunia (painful intercourse)
-
Dragging or drawing vaginal sensation
-
Urinary incontinence
-
Difficulty emptying bladder
-
Repositioning body to empty bladder
When there is break in the pubocervical fascia there is a loss of support of the urethra and/or bladder resulting in:
Cystocele: Loss of support at the level of the bladder. "bladder drop". This can be associated with loss of support of the urethra (cystourethrocoele) (Figure 1)
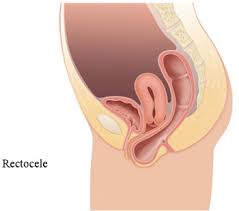
Posterior Vaginal Wall Prolapse (Rectocele)
The supportive layer of the posterior vaginal wall is called the rectovaginal septum or rectovaginal fascia. It is attached distally to the perineal body, laterally to the levator ani muscle and proximally to the cervix (if uterus is present). When a break in the rectovaginal septum is present the rectal wall will come into contact with the vaginal skin and create a bulge on the posterior bottom side of the vagina (Figure 2). The bulge will usually increase in size with bearing down (Valsalva maneuver) especially when having a bowel movement. Patients with a rectocele may experience:
-
Vaginal pressure/discomfort
-
Protrusion coming from the posterior vaginal wall
-
Difficulty evacuating rectum
-
Dyspareunia (painful intercourse)
-
Repositioning of body during bowel movements
Figure 2: Rectocoele (side view) - Note the break in the support structure known as the rectovaginal fascia. A break in the rectovaginal fascia allows the rectal wall to push directly against the vaginal epithelium (skin), thus creating a bulge or a rectocoele.
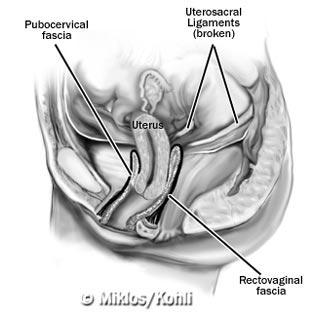
Uterine Prolapse
The uterosacral ligaments primarily support the upper 20% of the vagina (apex) and the uterus. When the uterosacral ligaments break the uterus begins to descend into the vagina (Figure 3 and 4). Further uterine descension pulls the rest of the vagina down resulting in apical tears of the anterior (pubocervical) fascia and posterior (rectovaginal) fascia from its points of lateral attachment. Anterior vaginal wall lateral tears are called paravaginal defects and results in cystourethrocele. Continued uterine and vaginal prolapse can result in a complete uterine and vaginal prolapse such that the uterus falls outside the vaginal opening and the vagina falls inside out.
-
Vaginal pressure/discomfort
-
Protrusion coming from the posterior vaginal wall
-
Difficulty evacuating rectum
-
Dyspareunia (painful intercourse)
-
Repositioning of body during bowel movements
Vaginal Prolapse Relaxation (continued)
Vaginal Vault Prolapse
Vaginal vault prolapse usually refers to an apical vaginal relaxation in an individual who no longer has a uterus (post hysterectomy). As the apex of the vagina continues to descend it pulls the rest of the vagina down resulting in apical tears of the anterior and posterior fascia from its lateral points of attachment. Continued descent of the vaginal apex may result in complete eversion of the vagina. Complete eversion of the vagina means that the once highest point in the vagina is now the lowest point hanging out of the vagina.
Prolapse Relaxation Figure: 1 - Normal support - vagina apex
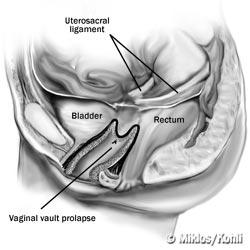
Vaginal vault prolapse - Loss of support of the uterosacral ligaments.
Vaginal Prolapse Relaxation (continued)
Enterocele
Enterocele occur primarily in patients who have had their uterus removed (hysterectomy). The anterior vaginal wall (pubocervical) fascia and posterior vaginal wall (rectovaginal) fascia separate and intestines can push directly against the vaginal skin. The herniation at the apex of the vagina is known as an enterocele.
Patients with a large enterocele, vaginal vault prolapse and uterine/vaginal prolapse may experience:
-
Pelvic or vaginal pressure
-
Difficulty evacuating rectum
-
Difficulty emptying bladder
-
Dyspareunia (painful intercourse)
-
Lower back pain/discomfort
-
Increasing pain/discomfort with prolonged standing
-
Decreased pain/discomfort upon lying down
-
Pain increases as day progresses
Pelvic Floor Exercises (Kegel Exercise)
Pelvic floor exercises are often taught to patients for treatment of urinary incontinence as well as vaginal prolapse. Though Kegel may be an effective treatment for fecal and urinary incontinence it has not been "proven" to be effective for prolapse. As described above, prolapse occurs due to a break in the fascia support system. Exercising the pelvic floor muscles will not put these breaks back together nor will it pull the prolapsed vagina, bladder, urethra, rectum, or uterus back into position. A simple analogy: a patient with an umbilical (belly button) hernia has a break in the supportive abdominal wall fascia…..all the sit-ups in the world may strengthen the abdominal wall muscles but will never put the abdominal wall fascia back together. However pelvic floor exercises may be useful especially when used in conjunction with a pessary. Pelvic floor exercises will strengthen the muscles of pelvic floor, and may enhance the ability to retain the pessary in the vagina.
Conservative Treatment of Prolapse
A pessary is a small device that can be inserted into the vagina to support the prolapsed vagina and its neighboring organs. This may relieve symptoms and reduce the prolapse, thus avoiding surgery. Many different types of pessaries are available for prolapse and urinary incontinence, some of which are shown below.

Surgical Options For Prolapse
Prolapse surgery is used to repair and reconstruct the support of the vagina and its neighboring organs when there is a prolapsed uterus. The surgeon's goal is to restore normal anatomy, sexual function and human physiologic function (urinating and defecating). Since uterine prolapse is not life threatening, surgery is indicated only if the patient feels that her condition is severe enough that it warrants correction. Mild prolapse need not be surgically corrected for it is rarely symptomatic. For further information about prolapse surgery, see the section under your operation.
Heavy Menstrual Periods (Menorrhagia)
Almost one third of women are affected by heavy menstruation at one stage in their lives. This can affect women of all reproductive ages, from teenagers to the age of the peri-menopause (the time period around the menopause). Some women also suffer from pain with their periods, and both can have a significant impact on quality of life. Women with heavy periods can also suffer from generailsed weakness and anaemia, with significant impact on work and family life.
I advise women initially to keep a menstrual diary to see if the pattern of bleeding is regular or irregular. For women above the age of 40, I take a small sample from the lining of the womb called endometrial biopsy (sample). This can normally be done in the outpatient clinic. In addition, I will organise for an ultrasound scan of the pelvis to assess the size of the uterus and the presence of fibroids, as fibroids can be an important cause of heavy bleeding.
For heavy regular periods, I advise women to try tablet treatment first that can reduce the heaviness of the bleeding with the period. If the bleeding pattern is irregular, it is important to try to regulate the periods with other tablets containing Progesterone (Norethisterone or Provera). These tablets can be taken from day 5 to day 21 of the period to stop the bleeding between periods.
If the above treatment fails, A medicated uterine contraceptive device called the Mirena IUD can be inserted (see picture). This contains Progesterone and releases it slowly in the womb to thin the lining of the womb and reduce the heavy menses. It normally takes up to 6 months to reach maximum benefit, during which women might experience irregular vaginal bleeding.
If the above conservative treatments failed, then I discuss surgical options for treatment of women with heavy periods, which include endometrial ablation and laparoscopic hysterectomy. For more detials see under "Your Operation".
Prolapse Surgery
Surgical options for patients with uterine and/or vaginal prolapse is dependent upon:
-
Degree or severity of prolapse
-
Areas specific for prolapse
-
Desire to maintain fertility (maintain uterus)
-
Desire to maintain sexual function
-
Patients age
-
Patients overall general health
-
Patients desire and opinion
Mr Fayyad has been trained to perform the prolapse repair procedures through multiple approaches such as:
Vaginally (through vagina)
Laparoscopically (mini-incisions) and Laparotomy (Large abdominal incision)
Mr Fayyad chooses to perform these procedures through the least invasive way possible for each individual patient.
In an attempt to restore vaginal anatomy, maintain sexual function and address urinary leakage, difficulty emptying bladder, and defecatory function, sometimes more than one surgical procedure are performed on the patient during one operation. This is done in an attempt at minimizing vaginal and uterine prolapse recurrence and therefore subsequent surgery.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on pelvic floor repair.
Laparoscopic Hysterectomy
As an advanced laparoscopic surgeon, Mr Fayyad performs total laparoscopic hysterectomy and laparoscopically assisted vaginal hysterectomy in women with heavy periods, painful periods and endometriosis. These procedures are now performed through 3 small abdominal incisions and the whole uterus is removed via key-hole surgery. The advantages for patients are immense, including one night hospital stay, quicker recovery and return to normal activiities including early return to work. In the days of modern surgery, this procedure should be the standard procedure for women who need hysterectomy for period abnormalities.
For further information about recovery following laparoscopic hysterectomy, please visit www.rcog.org.uk/recovering-well, and click on laparoscopic hysterectomy.
Anterior Repair
This procedure is performed in women suffering from prolapse of the front wall of the vagina (Figure 1). The procedure is performed under general anaesthetic, or spinal (epidural) anaesthetic. Occasionally it can be performed under local anaesthetic. The procedure involves putting your legs in stirrups, infiltration of the vaginal skin with local anaesthetic, followed by incision of the vaginal skin and the thin layer of muscle in the vagina. After that, the layer of muscle is brought together with a series of strong sutures and the vaginal skin is closed.
You will have a vaginal pack and catheter over night. The catheter will come out the next morning and you should be able to go home once you resumed normal voiding. The operation is generally safe, but occasionally women develop infection or bleeding after the operation. Also women may develop some difficulty passing urine initially. This tends to settle down with time. In 5-10% of the cases, the prolapse may come back needing further treatments. You may notice sutures coming out of the vagina in few weeks time. This is normal as your body is healing.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on pelvic floor repair.

Vaginal Hysterectomy
This procedure is performed in women with prolapse of the womb, to achieve good elevation of the top of the vagina. The procedure is done under general anaesthetic or spinal (epidural anaesthetic). It involves a cut in the vagina (not in the abdomen) followed by removal of the womb. The vaginal skin is closed afterwards and a pack and catheter inserted over night. They should come out in the next morning and you can expect to go home next day or the day after. We normally perform a repair operation at the same time of the hysterectomy. If you wish to avoid a hysterectomy, we have the unique expertise of providing key-hole prolapse surgery with preserving the uterus. See under laparoscopic uterine suspension (sacrohysteropexy).
For further information about recovery following this operation, please visit www.rcog.org.uk/recovering-well, and click on vaginal hysterectomy.
Posterior Repair
This procedure is performed in women suffering from prolapse of the back wall of the vagina (Figure 2). The procedure is performed under general anaesthetic, or spinal (epidural) anaesthetic. Occasionally it can be performed under local anaesthetic. The procedure involves putting your legs in stirrups, infiltration of the vaginal skin with local anaesthetic, followed by incision of the vaginal skin and the thin layer of muscle in the vagina over the prolapse. After that, the layer of muscle is brought together with a series of strong sutures and the vaginal skin is closed.
You will have a vaginal pack and catheter over night. The catheter will come out the next morning and you should be able to go home once you resumed normal voiding. The operation is generally safe, but occasionally women develop infection or bleeding after the operation. In 5-10% of the cases, the prolapse may come back needing further treatments. You may notice sutures coming out of the vagina in few weeks time. This is normal as your body is healing.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on pelvic floor repair.
Perineoplasty
This is an operation to tighten and rebuild the introitus (entrance to the vagina). Many women feel that the entrance to the vagina is loose which is mostly precipitated by childbirth. The operation involves approximating the muscles near the entrance to the vagina along with repair of the skin over it with sutures. You may experience pain following surgery, but this tends to settle down with time.
Mesh Vaginal Repairs
Mr Fayyad is one of few urogynaecologists in the UK performing mesh vaginal repairs for women with prolapse. Generally, the current indication is in women with recurrent prolapse (i.e. had previous prolapse treatment that did not work). Mr Fayyad uses the Prolift Total Mesh System in this select group of patients. Mr Fayyad has published his own experience in the use of this mesh system which is the longest follow up study currently published.

Laparoscopic Uterine Suspension
Traditional medicine recommends removal of the uterus (hysterectomy) when there is uterine prolapse. In cases of severe uterine and vaginal prolapse a hysterectomy followed by vaginal wall reconstruction may still be the most beneficial therapy. However there are more women who are electing to keep their uterus especially in those whom the uterus is only mildly or moderately prolapsed. The decision to attempt uterine and vaginal support is made only after a full informed consent is made with the patient having the operation. One of the most important aspects of this surgery is the lack of long term data supporting its utilization in uterine and vaginal prolapse surgery.
There are many methods of uterine suspension including sacrospinous tailbone) and uterosacral ligament suspension. Mr Fayyad routinely performs the laparoscopic approach and/or utilizing mesh to suspend the uterus (sacrohysteropexy Figures 1 and 2) or in some cases the uterosacral ligaments.
In the laparoscopic sacrohysteropexy with mesh, The cervix is grasped by special forceps (Figure 3). An incision is then made in the vaginal skin surrounding the cervix and a soft nylon mesh is then sutured to the cervix (Figure 4) and the vaginal skin closed over it (figure 5). The mesh is then secured to the sacrum (tailbone) through key-hole surgery (Figure 6) after reducing the prolapsed uterus. Then mesh is then buried using laparoscopic suturing techniques (Figure 8).
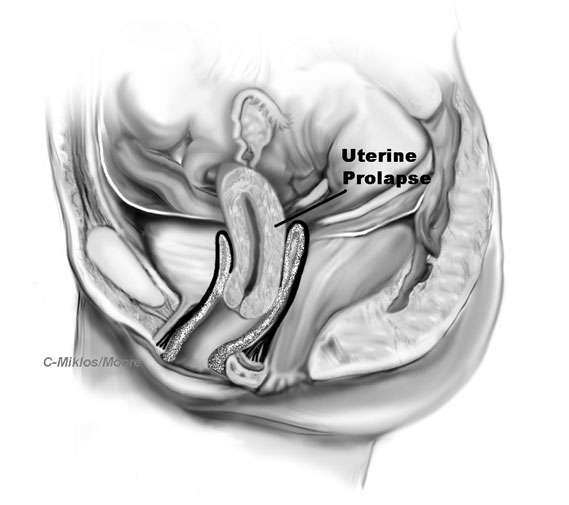
Figure 1: Diagrammatic presentation of uterine prolapse
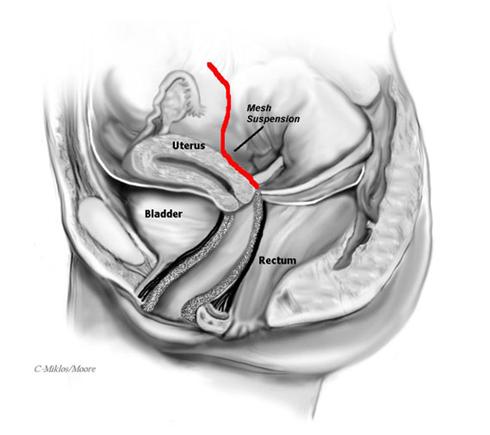
Figure 2: Sacrohysteropexy with mesh attaching the cervix to the sacrum
Laparoscopic sacrocolpopexy
The abdominal sacral colpopexy is one of the most successful operations for vaginal vault prolapse with excellent results. It involves suturing a synthetic mesh that connects and supports the vagina to the sacrum (tailbone). This procedure is complex in its nature and requires great expertise for a favorable outcome. Mr Fayyad has been performing the laparoscopic sacral colpopexy in the same manner as an open procedure with the exception of using a laparoscope over the past 5 years.
Advantages
By performing the sacral colpopexy laparoscopically, the vagina is repositioned to its anatomic position in a minimally invasive manner. Most surgeons perform this procedure through a large incision thus contributing to a longer recovery time. Our laparoscopic approach also allows us to incorporate additional laparoscopic procedures if needed.
Mr Fayyad can perform the laparoscopic sacral colpopexy in less time, less blood loss, smaller incisions and perform the surgery more precisely than by doing it through an open laparotomy. There are only very few centres in the country offering this procedure through the laparoscopic approach.
Surgical Technique for Laparoscopic Sacral Colpopexy
After placing two to three small incisions in the abdomen, the acces ports are placed, the bowel is mobilized out of the deep pelvis and the sacrum (tailbone) is identified. The peritoneum over the sacrum (tailbone) is elevated and then incised.
A vaginal probe is placed into the vagina to elevate the apex or vaginal vault into the surgical field.
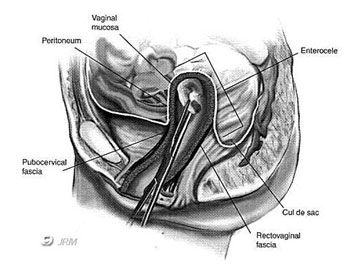
Figure 1 -- Vaginal vault (apex) : Probe holds vagina up from below
The peritoneum covering the apex of the vagina is incised and the bladder is dissected away from the top of the vagina anteriorly and the rectum dissected away posteriorly.
A piece of mesh which is shaped like a Y (Figure 5) is then attached both to the posterior aspect of the vagina, the vaginal apex and the anterior vaginal wall which normally supports the bladder. The mesh is then secured to the sacrum (tail bone) by strong staples (Figure 6).
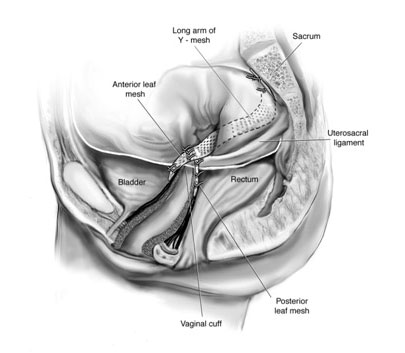
Figure 6- lateral view of mesh attached to the both anterior wall and posterior wall of vagina and then to the sacrum (tailbone)
Results/Complications
This procedure has excellent success rate with low complication rate. Some of the complications that can occur during Sacral Colpopexy include:
-
Mesh Infection
-
Mesh Erosion
-
Bleeding
-
Pain with intercourse
The most common risk of the use of mesh at the top of the vagina, is mesh extrusion through the vaginal skin, which is typically a minor complication, but one that does need a procedure to excise the exposed mesh and repair the skin where it came through. This risk exists whether the procedure is completed through an open incision or the laparoscope.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well, and click on pelvic floor repair and laparoscopy.
Sacrospinous Ligament Suspension
The sacrospinous ligament suspension fixation (SSLF) procedure is a less invasive and moderately successful operation for vaginal vault prolapse. This procedure is suitable for some patients that would not be candidates for laparoscopic or abdominal surgery or were felt to be better candidates for a vaginal approach under epidural anesthesia
The sacrospinous ligament technique is described below. Images are from Technique Spotlight Suture Placement, Vol. 3, by Boston Scientific featuring the use of the Capio (TM) Suture Capturing Device. The procedure is completed vaginally.
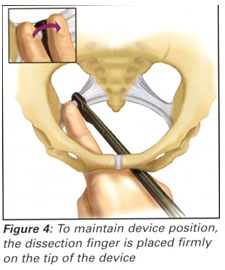
Sacrospinous Ligament Fixation Suture Placement
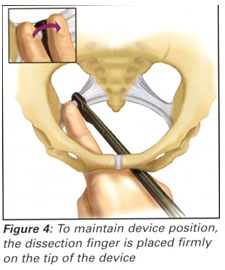
Vaginal Support with Sacrospinous Ligament Fixation
Results/Complications
This procedure should only be completed by experienced advanced pelvic surgeons. Risks include bleeding or hematoma in the pararectal or retropubic space (depending on posterior or anterior approach), injury or irritation to the pudendal nerve (buttock or leg pain).
As stated previously, many surgeons may not complete a vaginal vault suspension at the time of prolapse surgery, even if the patient has vault prolapse, because of the difficult and complex nature of the procedures reviewed above. This can lead to problems such as a shortened vagina, pelvic pain, painful intercourse, urinary symptoms (urgency, frequency, nocturia, difficulty emptying) that can occur post-operatively if the vaginal vault wasn’t properly suspended.
For further information about recovery following surgery, please visit www.rcog.org.uk/recovering-well and click on pelvic floor repair.