Laparoscopic Surgery
Defining Laparoscopy
The word Laparoscopy simply means visual examination of the abdomen by means of a laparoscope. Often called "belly button surgery", endoscopy, or keyhole surgery, it is a surgical technique involving small incisions in the abdomen through which major surgical procedures can be performed. One of the incisions of a laparoscopic procedure is made in the umbilicus ("belly button").
A laparoscope (something like a small telescope) is placed through this incision and attached to a small video camera. During the laparoscopic procedure, the video image is viewed on a television monitor in the operating room. Moving the laparoscope closer to the pelvic organs magnifies the area under investigation or operation. Laparoscopic surgery has been around since the 1850's and has evolved into a surgical technique used primarily for making diagnosis. In my experience, I utilize gynecologic laparoscopy in uterine removal as well as vaginal reconstruction and support of the bladder and the urethra.
Benefits of Laparoscopy
Cosmetic Benefits
Traditional types of surgery usually require large abdominal incisions. Laparoscopic procedures is usually performed through mini incisions.
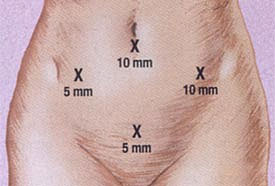
Laparoscopy - Entails making small incisions on the abdomen. Like the 4 small (all less than an inch) incisions seen above. Approximation (25mm = 1.0 inch)
Less Hospitalization
Most laparoscopic surgery cases are done as outpatient (Less than 23 hours). Major operations using a traditional incision (laparotomy) often require a hospital stay of 3-5 days
Quicker Recovery Time
Since laparoscopic surgery does not require the abdomen to be opened with a large abdominal incision, the patient takes less time to heal, requires less pain medication and is able to resume a more active lifestyle within a shorter period of time.
Decreased Scar Formation
Due to the small abdominal incision less internal scarring or adhesions can form. These adhesions can be a source of abdominal or chronic pelvic pain after laparoscopic surgery. Laparoscopy significantly reduces the scar formation (adhesions) and internal abdominal pain associated with these adhesions.
Laparoscopic Uterine Suspension (Laparoscopic sacrohysteropexy)
Traditional medicine recommends removal of the uterus (hysterectomy) when there is uterine prolapse. In cases of severe uterine and vaginal prolapse a hysterectomy followed by vaginal wall reconstruction may still be the most beneficial therapy. However there are more women who are electing to keep their uterus especially in those whom the uterus is only mildly or moderately prolapsed. The decision to attempt uterine and vaginal support is made only after a full informed consent is made with the patient having the operation. One of the most important aspects of this surgery is the lack of long term data supporting its utilization in uterine and vaginal prolapse surgery.
There are many methods of uterine suspension including sacrospinous tailbone) and uterosacral ligament suspension. Mr Fayyad routinely performs the laparoscopic approach and/or utilizing mesh to suspend the uterus (sacrohysteropexy Figures 1 and 2) or in some cases the uterosacral ligaments.
In the laparoscopic sacrohysteropexy with mesh, The cervix is grasped by special forceps (Figure 3). An incision is then made in the vaginal skin surrounding the cervix and a soft nylon mesh is then sutured to the cervix (Figure 4) and the vaginal skin closed over it (figure 5). The mesh is then secured to the sacrum (tailbone) through key-hole surgery (Figure 6) after reducing the prolapsed uterus. Then mesh is then buried using laparoscopic suturing techniques (Figure 8).
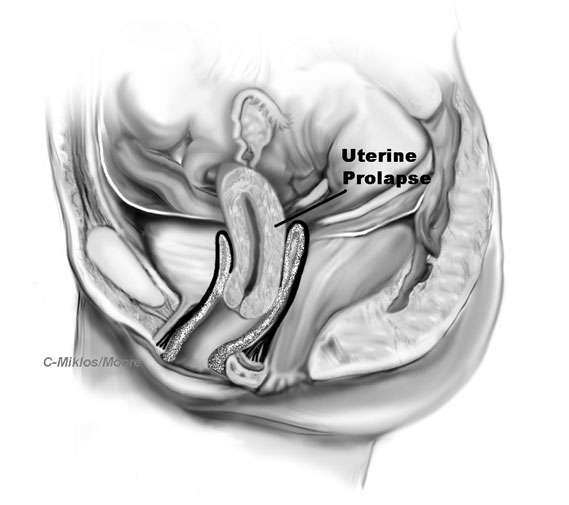
Figure 1: Diagrammatic presentation of uterine prolapse
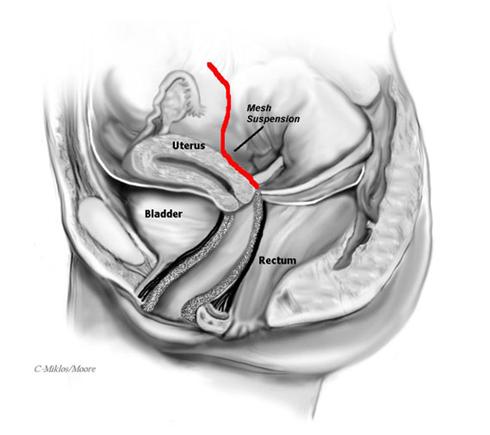
Figure 2: Sacrohysteropexy with mesh attaching the cervix to the sacrum
Vaginal Vault Suspension (Laparoscopic Sacrocolpopexy)
Overview
Vaginal vault prolapse occurs when the apex of the vagina (upper 1/3 of the vagina) has broken away from its original support structure known as the uterosacral ligaments. The uterosacral ligaments hold up the apex and the uterus when the uterus is in place (Figure 1). When a patient has a hysterectomy, the uterosacral ligaments must be cut to remove the uterus. In an attempt at preventing future vaginal apex or vault prolapse, the uterosacral ligaments should be attached to the apex of the vagina after the uterus has been removed.
If the patient did not have her uterosacral ligament attached to the vaginal apex or the uterosacral ligaments did not remain attached after the surgery, the patient risks ending up with vaginal vault prolapse after the hysterectomy (Figure 2). As the prolapse continues to pull down, it will increase the risk of anterior and posterior paravaginal defects.

Figure 1 Uterine & vaginal vault prolapse - The uterus begins to prolapse because of the broken uterosacral ligament.
IT IS VITAL THAT A VAGINAL VAULT SUSPENSION BE COMPLETED AT THE TIME OF PROLAPSE SURGERY IF VAULT PROLAPSE IS EVIDENT, WHICH IN MANY CASES IT IS.
Vaginal vault prolapse can also occur in many patients months or years after a hysterectomy in conjunction with other pelvic floor defects such as cystocele, rectocele, or enterocele. It is very important that the surgeon evaluates for vault prolapse in any patient presenting with prolapse, because in many cases what appears to the unexperienced examiner to be a cystocele or rectocele is actually vault prolapse. This misdiagosis leads to improper or incomplete repair and usually causes shortening of the vagina because the apex is not suspended up to its natural position. In many cases vault suspensions are not completed by some surgeons secondary to being more advanced difficult surgical procedures that require experience and training and therefore add considerable time to the procedure in inexperienced hands.
Symptoms such as urinary frequency, urgency, nocturia, abnormal emptying of the bladder and pelvic pain that may occur with vault prolapse or after prolapse surgery without vault suspension are relieved many times following proper vault suspension as seen in the below sections.
Indications
Patients that experience vaginal vault prolapse often feel pressure, pain, protrusion and/or dyspareunia (painful intercourse). There are different degrees of prolapse from mild to severe. If the prolapse is moderate or severe (extending outside the vagina), serious problems such as urinary retention, dilated ureter or kidney and vaginal ulcers may occur and surgery is the next step.
Indications for Surgery
-
Failure of Pessary Management
-
Symptomatic Prolapse (bulge, pressure, pain, dragging, discomfort)
-
Painful Intercourse
There are three many ways to perform vaginal vault suspension The most robust repair is laparoscopic sacrocolpopexy. Other options include sacrospinous ligament fixation and vaginal repair with mesh (Prolift TM). Mr Fayyad will discuss the surgical options after a complete physical examination and a discussion with the patient.
Laparoscopic sacrocolpopexy
The abdominal sacral colpopexy is one of the most successful operations for vaginal vault prolapse with excellent results. It involves suturing a synthetic mesh that connects and supports the vagina to the sacrum (tailbone). This procedure is complex in its nature and requires great expertise for a favorable outcome. Mr Fayyad has been performing the laparoscopic sacral colpopexy in the same manner as an open procedure with the exception of using a laparoscope over the past 5 years.
Advantages
By performing the sacral colpopexy laparoscopically, the vagina is repositioned to its anatomic position in a minimally invasive manner. Most surgeons perform this procedure through a large incision thus contributing to a longer recovery time. Our laparoscopic approach also allows us to incorporate additional laparoscopic procedures if needed.
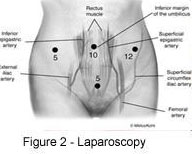

Mr Fayyad can perform the laparoscopic sacral colpopexy ( Figure 2 & 3) in less time, less blood loss, smaller incisions and perform the surgery more precisely than by doing it through an open laparotomy (Figure 1). There are only very few centres in the country offering this procedure through the laparoscopic approach.
Surgical Technique for Laparoscopic Sacral Colpopexy
After placing the four small incision sites noted above and then placing the access ports , the bowel is mobilized out of the deep pelvis and the sacrum (tailbone) is identified. The peritoneum over the sacrum (tailbone) is elevated and then incised. A sponge stick is placed into the vagina to elevate the apex or vaginal vault into the surgical field (Figure 2).
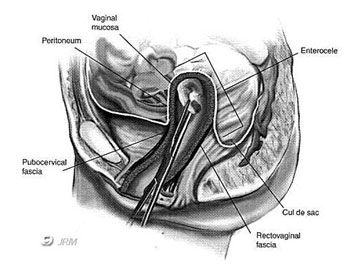
Figure 2 -- Vaginal vault (apex) : Probe holds vagina up from below
The peritoneum covering the apex of the vagina is incised and the bladder is dissected away from the top of the vagina anteriorly and the rectum dissected away posteriorly.
A piece of mesh which is shaped like a Y (Figure 3) is then attached both to the posterior aspect of the vagina apex and to the anterior vaginal apex.
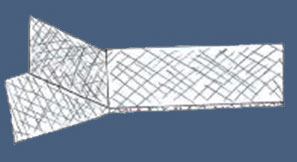
Figure 3 -- Y-shaped mesh
The long arm of the Y-mesh is then pulled up to the sacrum and subsequently attached. The mesh is secured with strong titanium staples into the sacrum, which will then be fixing the mesh. By attaching the mesh to the sacrum, the vagina is supported to the sacrum via a bridge of mesh between the vagina and sacrum (Figure 4).
The peritoneum, which was originally incised and opened at the beginning of the operation, is now closed over the mesh.This part of the surgery does not add support to the surgery but is thought to decrease potential complications, like bowel obstruction and adhesions.
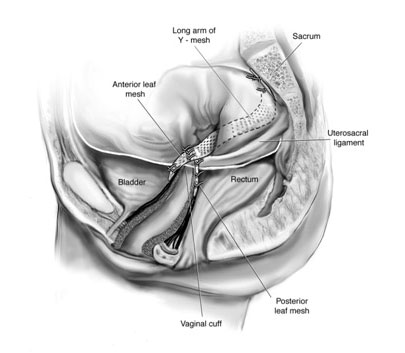
Figure 4- lateral view of mesh attached to the both anterior wall and posterior wall of vagina and then to the sacrum (tailbone)
Results/Complications
This procedure has excellent success rate with low complication rate. Some of the complications that can occur during Sacral Colpopexy include:
-
Mesh Infection
-
Mesh Erosion
-
Bleeding
-
Pain with intercourse
The most common risk of the use of mesh at the top of the vagina, is mesh extrusion through the vaginal skin, which is typically a minor complication, but one that does need a procedure to excise the exposed mesh and repair the skin where it came through. This risk exists whether the procedure is completed through an open incision or the laparoscope.
Total Laparoscopic Hysterectomy (TLH)
his is a new procedure where the hysterectomy is performed through key-hole surgery with substantial benefits to the patients’ recovery. Our Minimal Access Gynaecological Surgery Team led by Mr Fayyad routinely perform this procedure as one night stay procedure, with three small cuts in the abdomen, ranging between half and one centimetre. The procedure is done under general anaesrthetic with a small telescope introduced through the belly button. After wards, special fine instruments are introduced to cut the blood supply of the uterus using electrical energy and after separating the uterus from the bladder. Finally, a tube is introduced into the vagina and the uterus and cervix (neck of the womb) are removed in that tube coming out through the vagina. The last step of the operation involves closing the top of the vagina up using stitches introduced through key-hole surgery.
Generally, patients recover very quickly following this procedure with no abdominal scars, with substantial and swift recovery to normal activities.
Laparoscopic excision of endometriosis
Mr Fayyad routinely performs excision of endometriosis using key-hole surgery for patients with pelvic pain and pain during sexual intercourse. The procedure is performed using a small telescope introduced through the belly button. The endometriosis is removed using very fine instruments introduced through key-hole surgery.
Generally patients can recover very quickly, and patients are expected to go home the same day or stay for one night. Mr Fayyad, routinely performs complex procedures to remove endometriosis with varying degree of severity from mild to complex with extensive scarring and adhesions.